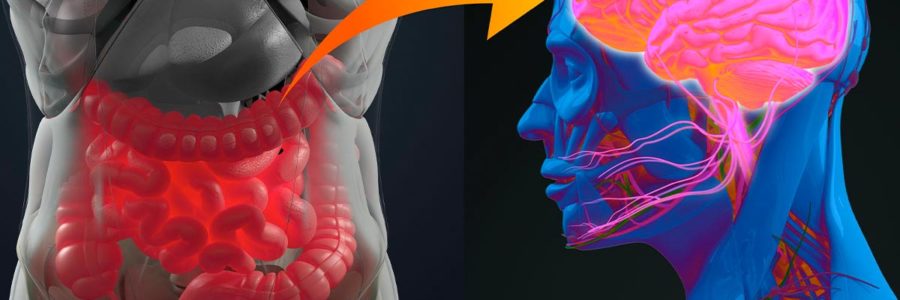
The Gut-Brain Connection: Gut healing has been at the forefront of the modern wellness world for good reasons. The gut is a significant player in many avenues of health, but it does not operate independently.
![]()
This article has been medically reviewed by Dr. Charles Penick, MD![]()
The gut-brain connection is well-documented, and yet many people don’t target the brain aspect of gut health. Today we explore the brain, how healing the brain heals the gut, and the top ways to optimize brain health.
Why Gut Health Matters
The gut plays an integral role in generating overall health. The gut does much more than facilitate digestion; much of the body’s immune system is located and developed in the gut. A healthy gut also communicates with the brain through nerves and hormones, enabling the body to operate correctly. When it comes to digesting food, the gut lining will also act as a barrier to entry, allowing the proper nutrients and keeping pathogens (like bacteria, fungi, or viruses) out.1
The Gut-Brain Connection: The Gut as the Second Brain
The gut is often referred to as the ‘second brain’ because of its influence on how the body functions. The enteric nervous system (which contains all the intestines) relies on the same type of neurons and neurotransmitters found in the central nervous system (which includes the brain and spinal cord).2
Many links have been made directly between the brain and the gut regarding symptoms. It is well-documented that stress directly impacts gut function.2-3 This cross-talk opens up the healing field and provides new ways to think about disease and healing.
Together, these “two brains” play a crucial role in specific diseases in our bodies and overall health. But, like anything, we tend to over-correct when there is a new discovery. The discovery of this ‘second brain’ has left many to put the real brain on the back burner, focusing entirely on the gut as a means to regain their health.
The Brain as the First Brain
Although the gut may be the second brain, we mustn’t forget that the brain is still the body’s maestro. The innate intelligence that the brain operates with controls the entire body via the central nervous system. The brain enables thoughts, memory, movement, and emotions through the nervous system by a complex function that is the highest product of biological evolution.4 Prioritizing a healthy brain during one’s life is the most crucial goal in pursuing health and longevity.
One of the central modulators between the gut-brain axis is the vagus nerve.5 The vagus nerve carries an extensive range of signals from the digestive system and organs to the brain and vice versa. It bypasses the spine and goes straight to the organs, including the gut.
This pathway plays a significant role in generating a sympathetic or parasympathetic state (whether you’re in fight and flight or rest and digest mode). It also influences how you digest and gut motility. What is called vagus nerve toxicity is when this pathway is now essentially shut down due to brain toxicity.5
Without getting this pathway back and running correctly, the body cannot detoxify, the gut functioning is impaired, there is chronic inflammation, and any progress you’ve made on your gut will eventually stall and then begin to worsen.
The Gut-Brain Connection: But My Brain Feels Fine?
The brain does not feel pain like the rest of the body because no nociceptors are located in the brain tissue itself. Studies explore various probings of the brain with no actual sensation in the brain itself, but rather showing up as referred pain in other parts of the body.6 Neurosurgeons can operate on brain tissue without causing a patient discomfort and can occasionally even perform surgery while the patient is awake.7
Although it may seem like your digestive issues are more pressing because you are aware of them, the reality is that everything stems back to the brain.
Symptoms of Brain Toxicity (Neurotoxicity)
Neurotoxins are toxic chemicals that attack nerves and the nervous system, the most significant source being the brain. Some of the common toxins that lead to neurotoxicity are mercury, aluminum, VOCs (like benzene, toluene, and xylene), conventional household cleaner ingredients (like diethanolamine (DEA), triethanolamine (TEA), alkylphenol ethoxylates (APEs), and propylene glycol), phthalates (found in plastic) and PVC (polyvinyl chloride).8
Symptoms of brain toxicity include:9
- Depression
- Anxiety
- Mood swings
- Memory problems
- Brain fog
- Irritability
- Confusion
- Sleep disorders
- Exhaustion
- Psychological distress
- Changes in touch or sensation
- Headaches
- Vertigo
- Coordination problems
- Digestive issues
- Numbness
- Pins and Needles feeling
As you can see, digestive issues and gut problems are but one of the many ways brain toxicity impairs the body. Returning to the source and fixing the root cause of toxicity will heal much more than just your gut.10
Symptom Management Vs. Fixing the Root Cause
Many people think that whenever they engage with a holistic modality, it addresses the root cause. This is not true. When it comes to the gut, all these ‘healing diets’ like the kinds that ban nightshades, oxalates, or lectins: these diets don’t address the root cause; they simply treat the symptoms.10-11
The goal should be to fix the problem and get to the root cause. When we look at this brain connection to the gut via the vagus nerve, we realize that if we’re not getting normal peristalsis– Yes, constipation’s a factor. Yes, SIBO is a factor, but we only can improve that peristalsis by enhancing the brain connection to the gut. You’ll never fix the microbiome when your detox pathways are backed up, and if your body is continuously dumping toxins in the gut, how are you going to improve the microbiome?
Removing trigger foods from your diet to relieve pain is a great short-term solution, but without going deeper and healing toxicity, what’s the point? These crazy elimination diets help relieve symptoms, but they are not sustainable and will never get your life back.
The Gut-Brain Connection: Should I Stop Working On the Gut All Together?
Although we have seen that the gut is downstream of the brain in terms of the ‘root cause’ of dysfunction, you should not necessarily abandon ship downstream. The goal is to clear the pathways from the source so that toxicity can flow out of the body altogether.
If the gut supplements you are currently taking are helping manage your symptoms, then there is no harm in supporting the gut directly. At the same time, you start to focus on brain detoxification. Avoiding trigger and inflammatory foods is also a good idea while you focus on the brain to add more inflammation to the mix.10
Don’t get stuck in the probiotic trap, which takes one strain of probiotics long term. This can lead to narrowing your microbiome because a probiotic supplement often overloads the gut with only a few strains when the gut should have tens of thousands of species.12 If you are taking a probiotic, rotate them regularly. Opt for probiotic-rich foods like fermented foods (including sauerkraut or yogurt) when in doubt.
One of the easiest (and most accessible) ways to boost your microbiome is to get outside! We take on good bacteria from the environment we spend time in, so spending time in nature is a great way to diversify your microbiome.
Another valuable thing to support the gut while also working upstream is consuming prebiotics. Prebiotics, the non-digestible fibers that feed your existing bacteria, often work better than probiotics.13 Prebiotic foods include chicory root, dandelion greens, Jerusalem artichoke, garlic, onions, leeks, asparagus, and green bananas.
Multidimensional Healing
Although getting to the source of toxicity is paramount, it’s important to note that healing will always be multidimensional and therefore require a multi-therapeutic approach. We are all individuals, and our illness (and healing) story is physical, emotional, and spiritual.
There are so many tools out there, which is why working with a functional medicine practitioner is invaluable. Understanding the pillars of health can be done using the three-legged stool analogy that honors health as a product of managing:
- Stressors (Physical, Chemical, and Emotional)
- Gut/ Microbiome
- DNA bio-individuality
These pillars are supported by ancestral healing methods, including intermittent fasting, feast/ famine cycling, dietary variation, hot/ cold therapy, and exercise. There are many tools to fast-track healing and promote the body’s innate intelligence, including chiropractic-facilitated alignment of the upper cervical spine.13
The Gut-Brain Connection: Summary
Although healing the gut is in vogue right now, it’s important to remember that this ‘second brain’ is downstream of the first brain: the brain itself. Although methods like elimination diets and probiotic supplementation often breed short-term success, they are more symptom-management tools. Getting back to the source of brain toxicity and specifically healing cellular toxicity will enable the body’s innate intelligence to restore the gut and many other bodily functions.
Healing toxicity on a cellular level requires a multi-therapeutic approach and various modalities to support the body. The 5R approach to detox can be paired with multiple ancestral healing methods like intermittent and extended fasting, hot/ cold therapy, diet variation, and exercise. Managing all three legs of the ‘health stool’ is one way to keep on track with health and includes mindfulness around stress, the gut microbiome, and your bio-individual DNA needs.
Medical Disclaimer: This article is based on the opinions of The Cell Health team. The information on this website is not intended to replace a one-on-one relationship with a qualified healthcare professional and is not intended as medical advice. It is intended to share knowledge and information from the research and experience of the Cell Health team. This article has been medically reviewed by Dr. Charles Penick, MD, for the accuracy of the information provided. Still, we encourage you to make your own healthcare decisions based on your research and in partnership with a qualified healthcare professional.
References
- UC Davis Health, Public Affairs and Marketing. “What Is ‘Gut Health’ and Why Is It Important?” UC Davis Health, health.ucdavis.edu/health-news/newsroom/what-is-gut-health-and-why-is-it-important/2019/07.
- “Gut-Brain Connection: What It Is, Behavioral Treatments.” Cleveland Clinic, my.clevelandclinic.org/health/treatments/16358-gut-brain-connection.
- Foster, Jane A., et al. “Stress & the Gut-Brain Axis: Regulation by the Microbiome.” Neurobiology of Stress, vol. 7, 2017, pp. 124–136., doi:10.1016/j.ynstr.2017.03.001.
- Wang, Yongjun, et al. “What Is Brain Health and Why Is It Important?” Bmj, 2020, p. m3683., doi:10.1136/bmj.m3683.
- Breit, Sigrid et al. “Vagus Nerve as Modulator of the Brain-Gut Axis in Psychiatric and Inflammatory Disorders.” Frontiers in psychiatry vol. 9 44. 13 Mar. 2018, doi:10.3389/fpsyt.2018.00044
- “Deep Brain Stimulation.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 7 Aug. 2020, www.mayoclinic.org/tests-procedures/deep-brain-stimulation/about/pac-20384562.
- “Awake Brain Surgery.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 7 May 2019, www.mayoclinic.org/tests-procedures/awake-brain-surgery/about/pac-20384913.
- “Common Household Toxins to Avoid.” Bastyr University, 27 May 2011, bastyr.edu/news/health-tips/2021/01/5-common-household-toxins-avoid.
- “Toxic Mold Exposure and Other Toxins.” Treating Brain Toxicity & Brain Infection | Amen Clinics, www.amenclinics.com/conditions/toxic-mold-exposure-and-other-toxins/.
- Amen, Daniel G. Change Your Brain, Change Your Life: Revised and Expanded Edition. Piatkus Books, 2016.
- Tilden, J. H. Toxemia Explained: the True Interpretation of the Cause of Disease: How to Cure Is an Obvious Sequence: an Antidote to Fear, Frenzy, and the Popular Mad Chasing after so-Called Cures. Health Research, 1997.
- Bush, Zach. “Why Probiotics Don’t Always Work.” Zach Bush MD, zachbushmd.com/wp-content/uploads/2017/04/Why-Probiotics-Dont-Always-Work-EG-BB-edit.pdf.
- Bransford, Richard J., et al. “Upper Cervical Spine Trauma.” Journal of the American Academy of Orthopaedic Surgeons, vol. 22, no. 11, 2014, pp. 718–729., doi:10.5435/jaaos-22-11-718.