![]()
This article has been medically reviewed by Dr. Charles Penick, MD![]()
Microbiome and Hormone Health: Gut health has become a hot topic in the wellness world due to its profound influence on various health markers. Today we explore the microbiome and its particular impact on female hormonal health and balance.
Microbiome and Hormone Health: What Is The Microbiome?
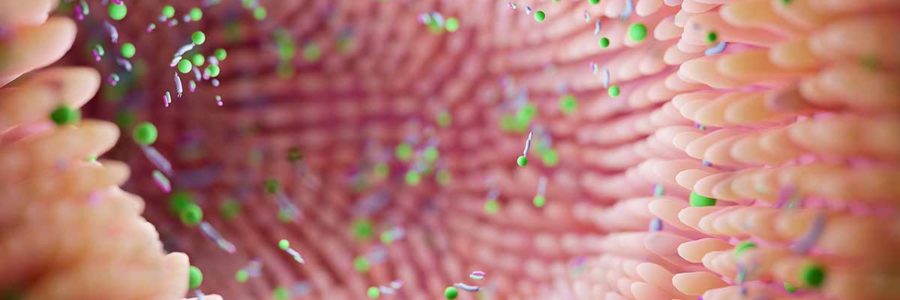
A microbiome is an environment that contains living bacteria. There are various types of microbiomes, including the human body biome as a whole or individual ecosystem within the body, like the skin biome, the mouth biome, and the gut biome.
Bacteria play a crucial role in generating our existence and health, for there are more bacterial cells in the human body than human cells. There are approximately 40 trillion bacterial cells to 30 trillion human cells.1,2 An optimally healthy gut should contain 20,000 – 30,000 different bacteria species. Most people living a modern “standard American” lifestyle include under 1,000 species.3
The human gut microbiome facilitates various bodily functions, including digestion, absorption, and assimilation of nutrients, immune regulation, brain health, and hormonal production.4-6 For this reason, having a microbially diverse gut is one of the most important aspects of maintaining whole-body health and longevity.
Microbiome and Hormone Health: The Microbiome Hormone Link
Hormones are signaling molecules that target organs to regulate physiology and behavior. The two main female hormones are estrogen and progesterone, which play a major role in metabolism and reproduction.7 Too much or too little of any hormone can dramatically affect the whole body.
Hormonal imbalances are prevalent in women; studies suggest that 80 percent of women suffer from hormonal imbalances. Symptoms of female hormone imbalances include:8-12
- Weight gain
- Fatigue
- Dry skin
- Constipation
- Overly cold or overly hot
- Muscle aches or tenderness
- Still joints
- Depression
- Low or no libido
- Infertility
- Sweating
- Thinning hair
The relationship between the gut microbiome and estrogen is deeply intertwined, with much cross-talk between the two. [13] The relationship impacts microbial diversity, estrogen metabolism and dominance, inflammation, and gut lining.
Microbiome and Hormone Health: Estrogen to Promote Microbial Diversity
Although estrogen is a significant player in reproductive health, it also plays a crucial role in various other functions. One such function is the promotion of growth and proliferation of good gut bacteria.13 When the gut bacteria is imbalanced (known as gut dysbiosis), genes and pathways are activated that negatively influence sugar and carbohydrate metabolism. One route, known as the TLR4 pathway, is linked to insulin resistance and an array of illnesses that can cascade as a result.14
Estrogen Metabolism and Dominance and Breast Cancer
Your gut microbiome plays a significant role in metabolism, which is important in keeping your hormones balanced. Female hormones fluctuate throughout the month, and estrogen can cause various problems when it is not metabolized well (known as estrogen dominance).
The gut biome breaks down estrogen by secreting an enzyme called β-glucuronidase. This enzyme breaks estrogen down into a free, biologically active form that can be taken up into the body’s tissues.15 And so gut dysbiosis can impair the process of estrogen metabolism, resulting in excess free estrogen levels not being appropriately used in the body.
One of the most lethal links between disease and excess estrogen in the body is hormone-dependent cancers, especially breast cancer, ovarian cancer, and endometrial cancer in women. As well as increased risk of blood clots and stroke.16
Although estrogen dominance is considered a hormonal imbalance with health consequences, estrogen itself is not ‘bad’ and has many critical roles in the body when in balance. Estrogen helps manage weight (especially abdominal fat) and promotes glucose tolerance when produced and metabolized properly.
Estrogen, Gut Lining, and Inflammation
When it is produced and metabolized correctly, estrogen helps reduce inflammation in the body and protect the integrity of the gut lining. It decreases the pathogenic populations of bacteria and the inflammation caused by lipopolysaccharide (or LPS).
LPS can interfere with the gut lining and cross the body’s gut barrier, causing a highly inflammatory response. Breaking down the gut lining, LPS can also open up the floodgates for all sorts of other inflammatory-causing invaders. Estrogen works to protect the integrity of the gut lining by eliminating LPS and has a preventative anti-inflammatory role.17
Maintaining the integrity of the gut lining is very important for overall health. This lining acts like a barrier between the outside world (pathogens, bacteria, viruses, and other inflammatory-inducing agents) and your body. Gut permeability (leaky gut) is linked to a wide range of disease models known to science, including Crohn’s disease, celiac disease, type 1 diabetes, type 2 diabetes, rheumatoid arthritis, spondyloarthropathies, inflammatory bowel disease, irritable bowel syndrome, schizophrenia, and certain types of cancer.18
Estrogen also helps produce a more robust gut lining because it is needed to form the gut’s epithelial layer and maintain a healthy, elastic, and tight junction.19 It prevents breakdown from lipopolysaccharides and helps strengthen the lining itself from unwanted molecules.
Microbiome and Hormone Health: Tops Ways To Improve Microbial Diversity in the Gut
Avoid Anti-Microbial Foods and Agents
Consuming good bacteria is only useful if you mindfully avoid the foods and other agents that kill bacteria. The anti-bacterial movement that swept the nation in favor of killing harmful bacteria does not selectively kill the bad. The good bacteria get bombed by using harsh anti-bacterial agents (like soaps, hand sanitizers, and antibiotics).20
Certain types of food and beverages target bacteria and make it very difficult for good bacteria to survive. They include artificial sweeteners, vegetable oils, and other PUFAs, alcohol.
Increase Consumption of Live Fermented Foods
Fermented live foods contain live probiotics and enzymes that can help increase the microbial diversity of your gut. [21] Aiming to consume at least one serving of fermented foods daily is ideal, but one serving per meal is optimal. Fermented foods include:
- Yogurt (unpasteurized)
- Kefir (unpasteurized)
- Kombucha
- Saurkraut
- Kim-Chi
- Beetroot kvass
- Miso
Increase Consumption of Prebiotic Foods
Prebiotic foods are rich in dietary fibers and sugars that feed the good bacteria in your gut. If probiotics are the seeds, then prebiotics is the soil, sunshine, and water that help bring them to life and keep them thriving. Prebiotic foods include:
- Leeks
- Dandelion greens
- Onions
- Garlic
- Jerusalem artichokes
- Chicory root
- Oats
- Barley
- Apples
- Bananas (especially green bananas)
Breathe in Microbes in Nature
One of the easiest and most profound ways to increase the microbial diversity in your gut is to spend time in nature, breathing in the air and getting exposure to the earth, trees, flowers, and dirt. Live microbes live abundantly in nature, especially in clean areas like national parks, the beach, larger forests, mountains, lakes, and creeks. Simply spending time in nature will introduce an array of healthy microbes into your body.3 So get outside!
Microbiome and Hormone Health: Summary
The gut microbiome plays a role in various bodily functions, including digestion, absorption, and assimilation of nutrients, immune regulation, brain health, and hormonal production. Microbial diversity has a cross-talk relationship with estrogen. Estrogen influences microbiome health and vice versa. Having a robust gut microbiome is vital to properly metabolize estrogen. Estrogen also plays a crucial role in keeping the gut lining healthy and robust. Some of the key ways to promote microbial diversity include: avoiding anti-bacterial agents and harmful foods, increasing your consumption of probiotics and prebiotic foods, and getting out in nature to breathe in healthy microbes.
Diversify Your Gut
There’s a problem with most probiotic pills and powders out there… Yes, even the ones that boast billions of CFU or colony-forming units. The problem is—most of these bacteria are dead. Others won’t survive the long and treacherous trip through your acidic digestive system and are mostly inert when they reach your gut.
That means many of the most expensive probiotics on your grocery store’s shelves aren’t doing anything at all.
That’s why I recommend a different kind of gut-boosting blend altogether—MegaSporeBiotic is a probiotic blend of 5 Bacillus spores that have been clinically shown to maintain healthy gut barrier function and overall immunity. In their spore form, they can withstand the acidic environment of your stomach by remaining dormant until they reach your GI tract. Once inside the large intestine, they transform into their active form and begin to colonize your gut.
If you’re searching for a way to quickly and effectively increase and balance microbial diversity, this is one of the best ways to do it.
> Check out MegaSporeBiotic now!
This article is based on the opinions of The Cell Health team. The information on this website is not intended to replace a one-on-one relationship with a qualified healthcare professional and is not intended as medical advice. It is intended to share knowledge and information from the research and experience of the Cell Health team. This article has been medically reviewed by Dr. Charles Penick, MD, for the accuracy of the information provided. Still, we encourage you to make your own healthcare decisions based on your research and in partnership with a qualified healthcare professional.
References
- Sender, Ron et al. “Revised Estimates for the Number of Human and Bacteria Cells in the Body.” PLoS biology vol. 14,8 e1002533. 19 Aug. 2016, doi:10.1371/journal.pbio.1002533
- Qin, Junjie, et al. “A human gut microbial gene catalog established by metagenomic sequencing.” Nature vol. 464,7285 (2010): 59-65. doi:10.1038/nature08821
- “Supplementation.” Zach Bush MD, 30 Jan. 2020, zachbushmd.com/probiotics/supplementation/
- Koenig, Jeremy E et al. “Succession of microbial consortia in the developing infant gut microbiome.” Proceedings of the National Academy of Sciences of the United States of America vol. 108 Suppl 1,Suppl 1 (2011): 4578-85. doi:10.1073/pnas.1000081107
- Rooks, Michelle G, and Wendy S Garrett. “Gut microbiota, metabolites, and host immunity.” Nature reviews. Immunology vol. 16,6 (2016): 341-52. doi:10.1038/nri.2016.42
- Cryan, John F, and Timothy G Dinan. “Mind-altering microorganisms: the impact of the gut microbiota on brain and behavior.” Nature reviews. Neuroscience vol. 13,10 (2012): 701-12. doi:10.1038/nrn334
- Seeman, Mary V. “Psychopathology in Women and Men: Focus on Female Hormones.” American Journal of Psychiatry, vol. 154, no. 12, 1997, pp. 1641–1647., doi:10.1176/ajp.154.12.1641.
- Turnbaugh PJ, Hamady M, Yatsunenko T, Cantarel BL, Duncan A, Ley RE, Sogin ML, Jones WJ, Roe BA, Affourtit JP, Egholm M, Henrissat B, Heath AC, Knight R, Gordon JI: A core gut microbiome in obese and lean twins. Nature 2009;457:480-484.
- Vitti, Alisa. Womancode: Perfect Your Cycle, Amplify Your Fertility, Supercharge Your Sex Drive, and Become a Power Source. HarperOne, 2014.
- Gottfried, Sara. The Hormone Cure Reclaim Balance, Sleep, and Sex Drive; Lose Weight; Feel Focused, Vital, and Energized Naturally with the Gottfried Protocol. Scribner, 2014.
- Seth, Bhavna, et al. “Association of Obesity with Hormonal Imbalance in Infertility: A Cross-Sectional Study in North Indian Women.” Indian Journal of Clinical Biochemistry, vol. 28, no. 4, 2013, pp. 342–347., doi:10.1007/s12291-013-0301-8.
- Ding, Sarah et al. “The Impact of Hormonal Imbalances Associated with Obesity on the Incidence of Endometrial Cancer in Postmenopausal Women.” Journal of Cancer vol. 11,18 5456-5465. 11 Jul. 2020, doi:10.7150/jca.47580
- Chen KL, Madak-Erdogan Z: Estrogen and Microbiota Crosstalk: Should We Pay Attention? Trends Endocrinol Metab 2016;27:752-755.
- Saad, M. J. A., et al. “Linking Gut Microbiota and Inflammation to Obesity and Insulin Resistance.” Physiology, vol. 31, no. 4, 2016, pp. 283–293., doi:10.1152/physiol.00041.2015.
- Baker JM, Al-Nakkash L, Herbst-Kralovetz MM: Estrogen-gut microbiome axis: Physiological and clinical implications. Maturitas 2017;103:45-53.
- Parida, Sheetal, and Dipali Sharma. “The Microbiome-Estrogen Connection and Breast Cancer Risk.” Cells vol. 8,12 1642. 15 Dec. 2019, doi:10.3390/cells8121642
- Sylvia, Kristyn E., and Gregory E. Demas. “Acute Intraperitoneal Lipopolysaccharide Influences the Immune System in the Absence of Gut Dysbiosis.” Physiological Reports, vol. 6, no. 5, 2018, doi:10.14814/phy2.13639.
- Bischoff, Stephan C et al. “Intestinal permeability–a new target for disease prevention and therapy.” BMC gastroenterology vol. 14 189. 18 Nov. 2014, doi:10.1186/s12876-014-0189-7
- Benedek G, Zhang J, Nguyen H, Kent G, Seifert HA, Davin S, Stauffer P, Vandenbark AA, Karstens L, Asquith M, Offner H: Estrogen protection against EAE modulates the microbiota and mucosal-associated regulatory cells. J Neuroimmunol 2017;310:51-59.
- Rangel, Gabriel W. “Say Goodbye to Antibacterial Soaps: Why the FDA Is Banning a Household Item.” Harvard University, 9 Jan. 2017, sitn.hms.harvard.edu/flash/2017/say-goodbye-antibacterial-soaps-fda-banning-household-item/.
- Ritchie, Marina L, and Tamara N Romanuk. “A meta-analysis of probiotic efficacy for gastrointestinal diseases.” PloS one vol. 7,4 (2012): e34938. doi:10.1371/journal.pone.0034938
This article is based on the opinions of The Cell Health team. The information on this website is not intended to replace a one-on-one relationship with a qualified healthcare professional and is not intended as medical advice. It is intended to share knowledge and information from the research and experience of the Cell Health team. This article has been medically reviewed by Dr. Charles Penick, MD, for the accuracy of the information provided. Still, we encourage you to make your own healthcare decisions based on your research and in partnership with a qualified healthcare professional.