Natural Solutions for Joint Pain: From subtle aches and stiffness when you first wake up in the morning to chronic conditions like osteoarthritis, joint pain can seriously disrupt your quality of life.

This article has been medically reviewed by Dr. Charles Penick, MD
More than fifteen million people report severe joint pain related to arthritis in the U.S., with 30.7 percent of adults aged 45 to 64 currently diagnosed.
Unfortunately, it’s far too easy to reach for over-the-counter medications for a quick fix instead of addressing underlying causes of joint pain. Pain relievers are not without side-effects and are simply a band-aid that can cover up the reason you have joint pain in the first place.
While there are multiple reasons why joint pain is so prevalent, addressing lifestyle, diet, and considering natural solutions is an essential first step for pain relief.
What causes joint pain in the body?
Regardless of the diagnosis, joint pain is related to inflammation. Inflammation can be caused by various modifiable factors, as you will learn below.
Inflammation is the body’s natural immune response to injury. It’s a way for your body to send out an SOS signal to the cells that help repair and restore damaged tissue or injuries.
However, with chronic joint pain, the inflammatory response doesn’t turn off because there is no resolution or repair. Your body keeps pumping out inflammatory mediators that can increase fluid, joint swelling, and even tissue damage. Addressing the reasons for inflammation may help calm this process, resulting in less pain.
What lifestyle factors can influence joint pain?
Anything that increases inflammation in the body can impact joint pain, so addressing overall inflammation in the body as a root cause is essential.
- Refined seed oils. Fats and oils like canola, soy, and corn are high in omega-6 fatty acids. Unlike the anti-inflammatory benefits associated with omega-3 fatty acids, omega-6 fatty acids have pro-inflammatory effects on the body. Because vegetable oils are so prevalent in the American diet, many people have an unhealthy ratio of omega-6 to omega-3, which impacts the inflammatory response.
- Food sensitivities. While you may associate food sensitivities with gut symptoms, joint pain can also be a sign. Food sensitivities can elicit an immune response in the body, releasing the same chemical mediators that lead to inflammation and pain. Additionally, joint pain is a common complaint from people with gluten intolerance or celiac disease. Addressing food sensitivities can influence and improve joint pain.
- Poor diet. Lack of fresh fruits, vegetables, and other fiber sources can significantly impact the body’s ability to regulate inflammation. As mentioned above, processed oils can increase inflammation in the body, but so can foods high in sugar, artificial sweeteners, and processed foods. Foods high in refined sugar can upregulate inflammation by impacting blood sugar balance—Oppositely, foods like fatty fish, cruciferous vegetables, and brightly colored berries all combat inflammation and free radical damage.
- Stress. Chronic stress means your body is in constant high gear, releasing chemical messengers that lead to inflammation.
- Overtraining. While we all know that physical activity is critical for a healthy lifestyle, overdoing it can put unnecessary wear and tear on your muscles and joints. Overtraining can increase inflammation in the body and even reduce your immune response.
Supplements for joint pain relief
While addressing the above lifestyle factors is critical to lower inflammation in the body, using natural supplements can be an option to reduce pain and address inflammation while avoiding medications with unwanted side effects.
Boswellia

Boswellia (commonly known as Frankincense) is a gum-extract that has been used in traditional medicine, especially Ayurveda. While many herbs have well-backed accounts of anecdotal evidence but lack published studies, Boswellia has published research for its anti-inflammatory benefits, especially for arthritis and joint pain.
Compounds in Boswellia may reduce specific pro-inflammatory cytokines that influence osteoarthritis, improving pain symptoms. One study found that supplemental Boswellia supported symptom improvement – including pain and physical function scores in as little as five days.
Turmeric

You may be more familiar with turmeric as a spice added to curries and soups, but the active compound curcumin is a well-known anti-inflammatory supplement. You’ll often find supplements with curcumin with added black pepper or lipids to improve intestinal absorption. Curcumin may turn down the inflammatory response related to pain by altering the release of inflammatory mediators.
While curcumin shows promise for overall inflammation markers in the body, there is significant research to support its benefits, specifically for joint pain. A study conducted on adults with pain from osteoarthritis found that curcumin helped both physical symptoms of pain and clinical markers of inflammation over eight months. Another study found that supplemental curcumin reduced scores for rheumatoid arthritis symptoms and CRP (a marker for general inflammation in the body). At the same time, the placebo group did not report improvements. Research also suggests that taking supplemental curcumin can reduce the use of NSAIDs for pain management.
Curcumin may also support a reduction in inflammatory markers related to exercise. A meta-analysis found that supplementation led to improvements in muscle soreness as well as markers of muscle damage.
N-Acetylcysteine (NAC)
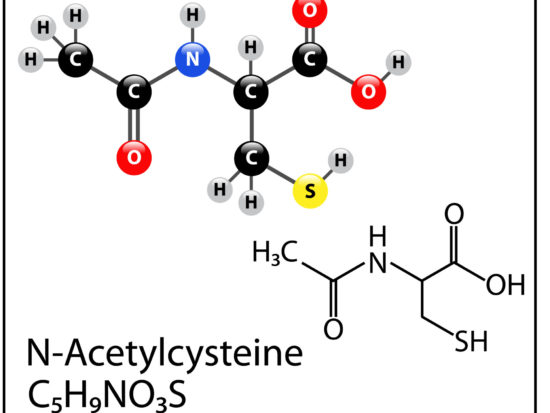
NAC is an amino acid precursor for glutathione production in the body. Glutathione is known as a master antioxidant in the body, buffering free radical damage that leads to oxidative stress.
Because it’s unclear how well supplemental glutathione raises levels in the body, supplemental NAC is used to increase production and reduce oxidative stress. In animal studies, NAC supported reductions in joint damage related to oxidative stress. Scientists suggest that oxidative stress may play a role in osteoarthritis and joint damage by damaging cartilage. This was also examined in a human study where NAC effectively decreased cartilage breakdown markers while improving pain and functional movement.
Another study found that adults with rheumatoid arthritis who took twice daily NAC supplements had significantly reduced inflammation markers compared to baseline and increased antioxidant measurements.
Addressing joint pain naturally.

While the causes of joint pain stem from various root causes, reducing overall inflammation in the body is an essential first step.
Focusing on lifestyle factors, including diet, movement, and stress reduction, are critical for addressing joint pain and overall wellness.
Natural supplements like Boswellia, turmeric, and NAC can support your pain-reduction plan, helping you avoid medications with unwanted side effects while focusing on adopting these healthy lifestyle changes.
Joint Support
Healthy joints start with targeted nutrients. But most people don’t get the nourishment they need for strong, pain-free joints as they age. And with countless “joint formulas” at your local health food store, it’s difficult to choose a supplement that actually works.
The secret to a good joint formula is a multi-layered approach to support. Systemic Formulas JOT-Joint, Disc, Cartilage Support is designed to support healthy joint function, lubrication, mobility, and comfort. With key nutrients like type II collagen (the best type for joint and muscle pain), MSM, and chondroitin, JOT contains all the nutrients you need for healthy joint function PLUS more.
One herb, in particular, has been used for thousands of years to reduce inflammation and decrease pain. And you won’t find this herb in many store-bought formulas…
>> Get JOT-Joint, Disc, Cartilage Support now and reclaim your pain-free life!
Medical Disclaimer: This article is based on the opinions of The Cell Health team. The information on this website is not intended to replace a one-on-one relationship with a qualified healthcare professional and is not intended as medical advice. It is intended to share knowledge and information from the research and experience of the Cell Health team. This article has been medically reviewed by Dr. Charles Penick, MD, for the accuracy of the information provided. Still, we encourage you to make your own healthcare decisions based on your research and in partnership with a qualified healthcare professional.
References
- “Joint Pain and Arthritis | CDC,” May 22, 2020. https://www.cdc.gov/arthritis/pain/index.htm.
- Sokolove, Jeremy, and Christin M. Lepus. “Role of Inflammation in the Pathogenesis of Osteoarthritis: Latest Findings and Interpretations.” Therapeutic Advances in Musculoskeletal Disease 5, no. 2 (April 2013): 77–94. https://doi.org/10.1177/1759720X12467868.
- Raphael, William, and Lorraine M. Sordillo. “Dietary Polyunsaturated Fatty Acids and Inflammation: The Role of Phospholipid Biosynthesis.” International Journal of Molecular Sciences 14, no. 10 (October 22, 2013): 21167–88. https://doi.org/10.3390/ijms141021167.
- Skodje, Gry I., Ingunn H. Minelle, Kjersti L. Rolfsen, Marina Iacovou, Knut E. A. Lundin, Marit B. Veierød, and Christine Henriksen. “Dietary and Symptom Assessment in Adults with Self-Reported Non-Coeliac Gluten Sensitivity.” Clinical Nutrition ESPEN 31 (June 2019): 88–94. https://doi.org/10.1016/j.clnesp.2019.02.012.
- López-Alarcón, Mardia, Otilia Perichart-Perera, Samuel Flores-Huerta, Patricia Inda-Icaza, Maricela Rodríguez-Cruz, Andrea Armenta-Álvarez, María Teresa Bram-Falcón, and Marielle Mayorga-Ochoa. “Excessive Refined Carbohydrates and Scarce Micronutrients Intakes Increase Inflammatory Mediators and Insulin Resistance in Prepubertal and Pubertal Obese Children Independently of Obesity.” Mediators of Inflammation 2014 (2014). https://doi.org/10.1155/2014/849031.
- Galland, Leo. “Diet and Inflammation.” Nutrition in Clinical Practice: Official Publication of the American Society for Parenteral and Enteral Nutrition 25, no. 6 (December 2010): 634–40. https://doi.org/10.1177/0884533610385703.
- Du, Chen, Amy Smith, Marco Avalos, Sanique South, Keith Crabtree, Wanyi Wang, Young-Hoo Kwon, Parakat Vijayagopal, and Shanil Juma. “Blueberries Improve Pain, Gait Performance, and Inflammation in Individuals with Symptomatic Knee Osteoarthritis.” Nutrients 11, no. 2 (January 29, 2019). https://doi.org/10.3390/nu11020290.
- Liu, Yun-Zi, Yun-Xia Wang, and Chun-Lei Jiang. “Inflammation: The Common Pathway of Stress-Related Diseases.” Frontiers in Human Neuroscience 11 (June 20, 2017). https://doi.org/10.3389/fnhum.2017.00316.
- Smith, Lucille Lakier. “Overtraining, Excessive Exercise, and Altered Immunity.” Sports Medicine 33, no. 5 (April 1, 2003): 347–64. https://doi.org/10.2165/00007256-200333050-00002.
- Syrovets, Tatiana, Berthold Büchele, Christine Krauss, Yves Laumonnier, and Thomas Simmet. “Acetyl-Boswellic Acids Inhibit Lipopolysaccharide-Mediated TNF-α Induction in Monocytes by Direct Interaction with IκB Kinases.” The Journal of Immunology 174, no. 1 (January 1, 2005): 498–506. https://doi.org/10.4049/jimmunol.174.1.498.
- Vishal, Amar A., Artatrana Mishra, and Siba P. Raychaudhuri. “A Double Blind, Randomized, Placebo Controlled Clinical Study Evaluates the Early Efficacy of Aflapin in Subjects with Osteoarthritis of Knee.” International Journal of Medical Sciences 8, no. 7 (2011): 615–22. https://doi.org/10.7150/ijms.8.615.
- Ramadan, Gamal, Mohammed Ali Al-Kahtani, and Wael Mohamed El-Sayed. “Anti-Inflammatory and Anti-Oxidant Properties of Curcuma Longa (Turmeric) versus Zingiber Officinale (Ginger) Rhizomes in Rat Adjuvant-Induced Arthritis.” Inflammation 34, no. 4 (August 2011): 291–301. https://doi.org/10.1007/s10753-010-9278-0.
- Jackson, J. K., T. Higo, W. L. Hunter, and H. M. Burt. “The Antioxidants Curcumin and Quercetin Inhibit Inflammatory Processes Associated with Arthritis.” Inflammation Research: Official Journal of the European Histamine Research Society … [et Al.] 55, no. 4 (April 2006): 168–75. https://doi.org/10.1007/s00011-006-0067-z.
- Belcaro, Gianni, Maria Rosaria Cesarone, Mark Dugall, Luciano Pellegrini, Andrea Ledda, Maria Giovanna Grossi, Stefano Togni, and Giovanni Appendino. “Efficacy and Safety of Meriva®, a Curcumin-Phosphatidylcholine Complex, during Extended Administration in Osteoarthritis Patients.” Alternative Medicine Review: A Journal of Clinical Therapeutic 15, no. 4 (December 2010): 337–44.
- Amalraj, Augustine, Karthik Varma, Joby Jacob, Chandradhara Divya, Ajaikumar B. Kunnumakkara, Sidney J. Stohs, and Sreeraj Gopi. “A Novel Highly Bioavailable Curcumin Formulation Improves Symptoms and Diagnostic Indicators in Rheumatoid Arthritis Patients: A Randomized, Double-Blind, Placebo-Controlled, Two-Dose, Three-Arm, and Parallel-Group Study.” Journal of Medicinal Food 20, no. 10 (October 2017): 1022–30. https://doi.org/10.1089/jmf.2017.3930.
- [16] Panahi, Yunes, Ali-Reza Rahimnia, Mojtaba Sharafi, Gholamhossein Alishiri, Amin Saburi, and Amirhossein Sahebkar. “Curcuminoid Treatment for Knee Osteoarthritis: A Randomized Double-Blind Placebo-Controlled Trial.” Phytotherapy Research: PTR 28, no. 11 (November 2014): 1625–31. https://doi.org/10.1002/ptr.5174.
- [17] Fang, Wang, and Yasaman Nasir. “The Effect of Curcumin Supplementation on Recovery Following Exercise-Induced Muscle Damage and Delayed-Onset Muscle Soreness: A Systematic Review and Meta-Analysis of Randomized Controlled Trials.” Phytotherapy Research: PTR, November 10, 2020. https://doi.org/10.1002/ptr.6912.
- [18] Pizzorno, Joseph. “Glutathione!” Integrative Medicine: A Clinician’s Journal 13, no. 1 (February 2014): 8–12.
- [19] Kasperczyk, Sławomir, Michał Dobrakowski, Aleksandra Kasperczyk, Alina Ostałowska, and Ewa Birkner. “The Administration of N-Acetylcysteine Reduces Oxidative Stress and Regulates Glutathione Metabolism in the Blood Cells of Workers Exposed to Lead.” Clinical Toxicology (Philadelphia, Pa.) 51, no. 6 (July 2013): 480–86. https://doi.org/10.3109/15563650.2013.802797.
- [20] Cornelis, Frederique M. F., Silvia Monteagudo, Laura-An K. A. Guns, Wouter den Hollander, Rob G. H. H. Nelissen, Lies Storms, Tine Peeters, Ilse Jonkers, Ingrid Meulenbelt, and Rik J. Lories. “ANP32A Regulates ATM Expression and Prevents Oxidative Stress in Cartilage, Brain, and Bone.” Science Translational Medicine 10, no. 458 (September 12, 2018). https://doi.org/10.1126/scitranslmed.aar8426.
- [21] Ozcamdalli, Mustafa, Abdulhamit Misir, Turan Bilge Kizkapan, Erdal Uzun, Fuat Duygulu, Cevat Yazici, and Ibrahim Halil Kafadar. “Comparison of Intra-Articular Injection of Hyaluronic Acid and N-Acetyl Cysteine in the Treatment of Knee Osteoarthritis: A Pilot Study.” Cartilage 8, no. 4 (October 2017): 384–90. https://doi.org/10.1177/1947603516675915.
- [22] Hashemi, Ghazal, Mahtabalsadat Mirjalili, Zahra Basiri, Ahmad Tahamoli-Roudsari, Nejat Kheiripour, Maryam Shahdoust, Akram Ranjbar, Maryam Mehrpooya, and Sara Ataei. “Evaluating the Effects of Oral N-Acetyl Cysteine on Inflammatory and Oxidative Stress Biomarkers in Rheumatoid Arthritis.” Current Rheumatology Reviews 14 (September 26, 2018). https://doi.org/10.2174/1573403X14666180926100811.


